In Rwanda, visionary doctor is moving mountains again
Health system built from the ground upBy Bella EnglishGlobe Staff / April 13, 2008
photo gallery >> Paul Farmer's mission in RwandaRWINKWAVU, Rwanda - It was November 2004, and Dr. Paul Farmer had agreed to bring his world-renowned Partners in Health model to Rwanda, which was still reeling from the aftershocks of the genocide a decade earlier. Now here he was, with Rwandan health officials, to scout out a location for a hospital to serve the poorest of the poor.
Farmer, who teaches at Harvard, was taken to Ruhengeri, in the country's northwest corner. But there was already a clean hospital there, with employees and even an X-ray machine. "No, no, no. You don't understand," Farmer recalls saying. "Find me the worst possible place in the country."
So they took him to Rwinkwavu, a remote area two hours east of Kigali. Even Farmer - who works in the world's worst regions - was taken aback. The "hospital" consisted of derelict buildings that had been used by a Belgian mining company decades earlier, then as military barracks during the genocide in which 800,000 people were killed in 100 days. Bullet holes pocked the walls, which were also scarred with hate messages left by the killers: "Those we don't kill, AIDS will get."
There were no beds, no patients, no staff, no medical equipment. "It was abandoned, dirty and scary," Farmer says. There were 200,000 people in the district and not a single doctor.
It was the perfect place for Farmer.
With the help of the Rwandan Ministry of Health and the Clinton Foundation, Farmer went in with American and Rwandan workers to rebuild the facility and find Rwandan doctors and nurses. During that time, he and Dr. Michael Rich, who was raised in Natick and is Rwanda country director for Partners in Health, and their colleagues lived in decrepit housing left over from the mining days. Over the years squatters had moved in, so Partners in Health - or "Inshuti Mu Buzima" in Kinyarwanda - had to start a housing program, too, constructing 120 concrete or brick houses, a huge improvement over the mud shacks that look as if they'd dissolve in a good rainstorm.
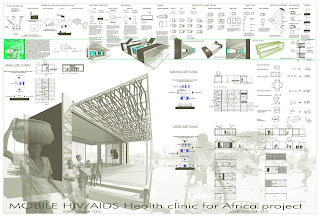
In the summer of 2005, the doors opened at Rwinkwavu Hospital, which now sees 250 patients a day, some of them walking hours to get there. Farmer, Rich, and their Rwandan counterparts have built a second hospital in an equally remote area of 200,000 - also without a single doctor - and built or renovated 19 health centers that feed patients to them. A third hospital is on the drawing board, designed by Harvard architecture students. Ultimately, they plan to expand rural medical services to the entire country.
Reluctant heroFive years ago, Farmer became reluctantly famous with the publication of Tracy Kidder's best-selling book, "Mountains Beyond Mountains," which told the story of the brash Harvard Medical School graduate who changed the face of healthcare in rural Haiti. Now 20 years old, Partners in Health, with its emphasis on treating poverty as well as disease, has expanded to nine countries.
Though Haiti will always be his "true north," as Farmer puts it, it had become too dangerous there to raise a family. Rwanda is today considered quite safe under the presidency of Paul Kagame, the former rebel leader who stopped the genocidal slaughter that erupted 14 years ago this month. Farmer, a Harvard professor who each fall teaches undergraduates and medical students about global health issues and infectious disease, has moved with his family to Rwanda, where he recently became a citizen and a member of the Rwandan Medical Society. He'll be in Boston later this month for speaking engagements at MIT, Harvard Medical School, and a Brookline church.
His wife, Didi, who is Haitian, has a degree in medical anthropology and spends half the week with Farmer at Rwinkwavu, where she runs the community health workers program. The couple live with several other Partners workers in a modest house on the grounds. The rest of the week they spend at their rental home in the capital of Kigali, where their 10-year-old daughter, Catherine, attends private school.
The Farmer family recently welcomed two new members: Elizabeth, 6 months old, and Sebastian, born in February. Elizabeth was abandoned at Rwinkwavu as a newborn, and Didi, who was pregnant at the time, called and asked her husband if they could take her in. Though Rwanda does not encourage adoption, the government approved it.
"I had no criminal record, and I was under 50," quips Farmer, who is 48.
The truth is, Partners in Health has an excellent relationship with Kagame's government. "Our vision matches theirs," Farmer told a group of Americans who toured Rwinkwavu in early March. On this particular day, he is wearing a loud shirt with a busy African pattern on it, sewn by a grateful patient. "In Haiti, they give me potatoes and carrots," he says. Here, it's a handmade item of some sort for no one has money and Partners In Health services are free.
He tells his audience that Rwanda is the perfect place for his organization. "This is the most exciting thing I've seen in 25 years. Here we're in a country that came from a terrible place and in just 12 years says it wants a national health program with 40,000 to 50,000 health workers." Because of the government's commitment, Rwanda's progress on HIV/AIDS has been remarkable, with less than 3 percent of the population infected.
The third partner is the Clinton Foundation, the former president's organization dedicated to addressing health inequalities in developing countries. While Partners provides the medical expertise, the foundation provides funding, management, and policy support. The two groups also run programs together in Lesotho and Malawi. Farmer and Rich are paid by the Brigham and Women's Hospital, which also sends medical residents to work with them and learn about global health. The program manager for Rwanda is another New Englander: Melissa Gillooly from Warwick, R.I., who also lives on the hospital grounds.
With a $50 million annual budget spread over nine countries, Partners stays barely three months ahead in funding, which keeps Farmer up at night. "I go to bed worrying about all the promises we've made," he says, "and I get up each morning thinking we haven't made enough promises."
Dignity amid povertyThe countryside en route to Rwinkwavu Hospital is lush with banana groves, eucalyptus forests, and deep emerald valleys with sweeping views of the mountains. Rwanda is known as "The Land of a Thousand Hills," which seems a gross undercount. It is indeed a land of mountains beyond mountains.
But the close-up view from the Toyota pickup that Farmer is driving on a recent weekday is not so pretty. Everywhere there are mud huts with dirt floors and no electricity, water or toilets. Straight-backed women carry huge cans of water on their heads, while stooped men push bicycles overloaded with stacks of wood or bunches of bananas.
Everywhere, there are children; Rwanda, the size of Maryland, is Africa's most densely populated country. Big children hold small children; small children hold toddlers. Babies are bound to their mothers' backs with colorful cloth, even as they bend over in fields.
The bumpy secondary road ends at Rwinkwavu Hospital, and the unbaked scenery instantly changes. Bauhinia trees bloom along with bignonia vines and creeping ficus, set among several low buildings.
In the middle of the hospital grounds is a fish pond, a Farmer trademark at all Partners clinics. He and his brother Jeff, a former professional wrestler, dug this pond themselves, wading into swamps for plants and fish. Farmer says it's about providing dignity and something of beauty to the poor.
The 96-bed hospital includes a pediatrics and a malnutrition ward, operating room, women's clinic, radiology, pharmacy, dental clinic, lab, and a lively center for children with HIV/AIDS.
A field of soybeans flourishes on the grounds; the hospital lends the land to farmers with HIV/AIDS. Just beyond is the start of a training center for medical workers in Rwanda and throughout Africa. A nearby dorm for visitors has just been completed.
At the hospital, each bed has a mosquito net hanging above. In pediatrics, the first bed in the ward holds a preemie so tiny it's hard to tell she's even there. Other beds are filled with children suffering from septic shock, a brain tumor, malaria, and heart problems. Their mothers rarely leave their side.
Next door, the malnutrition ward is eerily quiet considering all the babies and toddlers, most of them lethargic. When patients are discharged, they go home with food and follow-up from local health workers hired and trained by Partners.
It is these "accompagnateurs" - neighbors, really - who are the backbone of Partners in Health. They go into homes to check on discharged patients and identify others at risk. They also visit those with chronic illnesses such as HIV/AIDS to make sure they're taking their medications, and to provide company. Partners is by far the biggest employer in their local areas: 1,500 so far, including 825 community health workers.
"Good things happen when you create jobs," Farmer says. The accompagnateurs, some of them HIV-infected themselves, can now support their own families. And the visits are healing, Farmer believes: "It's not so much about supervising as it is about being neighborly."
Rising above the past"Neighborly" is a loaded word in this country, where the majority Hutu butchered the Tutsi and moderate Hutu during the genocide. Neighbors killed neighbors, teachers and students killed each other, workers killed co-workers, doctors killed patients, priests killed parishioners - and vice versa. Many Partners staffers are Tutsi, while most of the patients, because they comprise 85 percent of the population, are Hutu. Thus, many Tutsi workers are treating Hutu patients and, under the housing program, building homes for Hutu families.
Bruce Nizeye was 14 years old when the genocide broke out. He watched as his father was taken away and shot to death. His 18-year-old brother was killed at school. The family house was burned down. Two years later, Nizeye found his mother in a refugee camp.
Now 28, he works with Farmer, who was best man at his wedding. ("I gave him a cow as a gift," Farmer says. "It's traditional for best man.") Like his father, Nizeye is an engineer, and directs Partner's building program. That means he has built many houses for Hutus, the group that torched his childhood home. Indeed, some of them may have destroyed the very homes they are helping rebuild.
Nizeye is also in charge of renovating the dilapidated infirmary at the country's largest prison, which Partners took on when Farmer learned there was no doctor for its 10,000 inmates. At the prison, Nizeye's workers are mostly the incarcerated "genocidaires."
Does it bother him to work with, and for, the people who killed his loved ones and destroyed his home?
"I don't even ask," Nizeye says. "I ask if someone is a hard worker or doing his job well, not if he is a Hutu."
At Rwinkwavu, Nizeye has jumped into the pickup with Farmer for the 45-minute trip to a Partners clinic in Rukira over deeply rutted roads that are little more than paths. Farmer maneuvers around a dead cow and picks up a couple of hitchhikers, when Nizeye gives the nod.
At Rukira, abundant flora - bignonia vines, bougainvillea, cala lilies - and a fish pond once again grace the grounds, while patients and relatives wait in shaded areas. Farmer is there to discuss a complicated case with the center director, and to see another patient who was raped and bayoneted during the genocide and is HIV-positive. Sometimes, he'll treat a hippo bite or land mine injury.
Back at Rwinkwavu, Claire is lying in wait for him. At 24, she has cared for two younger sisters for years, since their parents died from AIDS. Claire is also infected. She's a patient of Farmer's, but this day has other business. She wants a job. Though Farmer has a long list of patients, doctors, and staffers waiting, he sits down and looks at her resume.
"What do you want to do with your life. What is your dream?" he asks.
"I want to get a job and take care of my sisters," she replies.
"That's not a dream, that's a necessity," he says. They talk a bit about her dreams, and he promises to see what he can do.
Next, he stops by the lab to get some test results. He shakes his head: "Not good." Everywhere, he greets patients who ask about his new baby. "Bonjour, mon frere," "Bonjour, ma cher," he says, exchanging the Rwandan triple cheek-kiss. Some back-packing Brit with time on his hands has shown up unannounced to visit the doctor. Farmer is polite, but he's got work to do.
In the pediatrics ward, he and Dr. Jean Bosco Niyonzima head to Bed 6, where a young mother sits with her listless toddler. Farmer, speaking French, questions the mother, while Bosco translates into Kinyarwanda. When the woman says she has lost her two other children to disease, Farmer winces.
"Tell her the boy looks good, I don't want her to panic," he says. He suspects tuberculosis.
More to doIt's 5:30 p.m., and Farmer hasn't had lunch. His day started before 7 a.m. in Kigali, when he dropped Catherine at school. He and Gillooly attended a meeting with Rwandan health officials before setting off for Rwinkwavu, with a stop at the prison, Rwinkwavu Hospital, Rukira health center, and back to Rwinkwavu.
Now, Farmer and Rich are anxious to take their periodic power-walk up a nearby mountain. They are also anxious about their work, especially the ambitious expansion of the Partners model to all 27 districts and 9 million residents of rural Rwanda, in partnership again with the Ministry of Health and the Clinton Foundation. Right now, only a couple of dollars a year is spent on each rural patient in Rwanda; the doctors want to increase that tenfold. (The United States spends nearly $7,000 per person.)
"We want to be an organization that says yes," Farmer says. "We have to find some big donors." His work in Rwanda, he says, will take at least 10 more years.
Why does he do it all?
"Because it works, because it's exciting, because we're working hand-in-hand with the government. Plus, treating a hippo bite is really cool."
Paul Farmer will deliver the keynote address Saturday at an MIT conference organized by Global Poverty Initiative. On April 22, he will speak at the Harvard School of Public Health with Dr. Agnes Binagwaho, head of Rwanda's National AIDS Control Commission. On April 27 he will receive the 2008 Spirituality and Justice Award and deliver a sermon at All Saints Parish in Brookline.
© Copyright 2008 Globe Newspaper Company.